Antimicrobials in aged care

Recent work by the Australian Commission on Safety and Quality in Health Care — as part of the Antimicrobial Use and Resistance in Australia (AURA) Surveillance System on antimicrobial resistance (AMR) and antimicrobial prescribing in Australian residential aged-care homes — has delivered a powerful reminder that action to improve antimicrobial use is vital to the safety of residents.
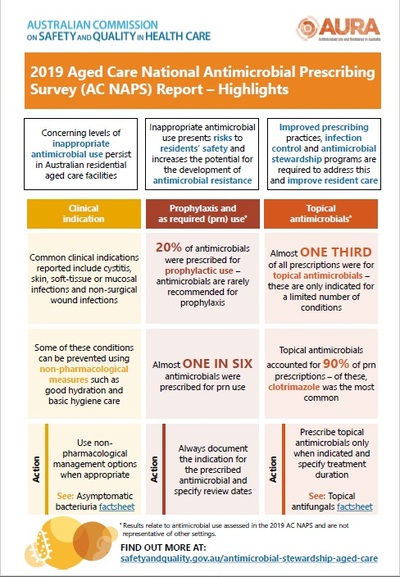
Strategies to improve antimicrobial prescribing and reduce the risk of inappropriate antimicrobial use among older patients are key to combating antimicrobial resistance. These strategies include reducing the number of prescriptions for prophylaxis (which is rarely recommended) in aged-care homes; continuing to improve documentation of antimicrobial prescriptions; and considering better use of preventative measures, such as non-pharmacological management of some clinical indications, such as cystitis, skin and wound infections.
As part of the AURA Surveillance System, the Commission has recently published the 2019 Aged Care National Antimicrobial Prescribing Survey (AC NAPS) Report, in conjunction with the National Centre for Antimicrobial Stewardship. The 2019 AC NAPS Report provides information on infections and antimicrobial use for 32,347 aged-care residents from 568 Australian residential aged-care services.
The 2019 AC NAPS data demonstrate ongoing and concerning levels of inappropriate antimicrobial use in Australian residential aged-care services, with implications for the safety of residents. In combination with the prevalence of antimicrobial resistance in the community, this inappropriate use of antimicrobials creates the potential for amplification of antimicrobial resistance in this vulnerable population.
As shown in AURA 2019 — the biennial report on antimicrobial use and resistance in Australia — some multi-resistant organisms such as strains of Escherichia coli and methicillin-resistant Staphylococcus aureus are already prevalent in aged-care facilities.
Antimicrobial use in aged-care services is a critical area for service improvement, given older people may have regular hospital admissions and be more susceptible to infections due to their close living environment, being immunocompromised and greater use of invasive devices. They are also more likely to take multiple medications, so the burden of adding antimicrobials for these patients is high. Antimicrobials are not without safety risks and adverse effects such as renal impairment and Clostridiodes difficile can be more significant in the elderly population.
The AURA Surveillance System also includes Australian Passive AMR Surveillance (APAS), which provides data showing that aged-care homes experience high rates of multidrug-resistant infections such as Escherichia coli. The Aged Care Quality and Safety Commission’s Aged Care Quality Standards also specifically mention the promotion of appropriate antimicrobial prescribing.
The Australian Commission on Safety and Quality in Health Care is currently working with, and supporting, the Aged Care Quality and Safety Commission, multi-purpose services, aged-care providers and general practitioners who work in aged-care homes, to promote antimicrobial prescribing improvement programs informed by the AC NAPS findings.
Ongoing surveillance of infections and antimicrobial use will remain important in informing residential aged-care providers’ strategies for improving care. Strategies to improve resident safety include:
- Regularly reviewing usage patterns, in collaboration with medical and nursing staff, including prescriptions for antimicrobial prophylaxis, and compliance with Australian Therapeutic Guidelines on recommended duration and choice of antimicrobials.
- Sharing analyses of AC NAPS data with administrators, governance groups and clinicians such as general practitioners, pharmacists and nurses, to develop targeted improvement strategies.
- Reflecting on how results from AC NAPS data are communicated to clinicians, governance and leadership groups, residents and their families.
- Using medication charts consistent with the Commission’s National Residential Medication Chart to improve documentation.
- Implementing policies that require default, fixed-length courses of treatment and mandatory review dates, particularly for ‘when required’ prescriptions.
- Engaging external expert support for aged-care staff on antimicrobial use, and diagnosis, prevention and control of infections, as required.
- Using resources to support implementation of policies and procedures consistent with the Australian Guidelines for the Prevention and Control of Infection in Health Care.
- Introducing infection prevention and control, and antimicrobial stewardship education for nurses, prescribers and family members of residents to raise awareness and skill levels.
- Offering education for non-nursing staff who provide care to residents on the importance of infection prevention and control and basic personal and hygiene care.
Key findings from the AC NAPS 2019 Report
- Approximately 20% of prescriptions were for prophylaxis, which is concerning as antimicrobials are rarely recommended for prophylaxis.
- Almost one-third (30.4%) of all prescriptions were for topical antimicrobials, which also accounted for more than 90% of prn (as required) prescriptions, most commonly clotrimazole (74.1%). The prn use of clotrimazole may lead to inappropriate duration of therapy, and unnecessary use of antifungals, either topically or systemically, which may contribute to the development of resistance.
- Almost one in six (15.0%) antimicrobials were prescribed for prn administration, which may reduce clinical review of antimicrobial choice at time of onset of infection and decisions regarding duration of treatment, leading to extended duration of treatment.
- There was an improvement in documentation of antimicrobial review or stop dates (64.7%) compared with 2018 (58.9%).
- The most common clinical indications for antimicrobial use were cystitis; other — skin, soft tissue or mucosal; pneumonia; tinea; and non-surgical wound infections. Many of these conditions can be prevented by managing hydration and providing good basic hygiene care. Non-pharmacological management is also a key consideration for these conditions.
- Cefalexin, topical clotrimazole, amoxicillin–clavulanic acid, trimethoprim and doxycycline were the most commonly used antimicrobials. Agents with narrower spectrums than cefalexin and amoxicillin–clavulanic acid are recommended for many infections, as they are less likely to promote antimicrobial resistance.
As topical antifungal use and unnecessary treatment of asymptomatic bacteriuria are two persistent issues identified from AC NAPS, resources have been developed to support responses to these issues.
Access current resources to support antimicrobial stewardship in aged-care settings at: https://www.safetyandquality.gov.au/antimicrobial-stewardship-aged-care.
Could slow water flow be risky when handwashing?
The speed at which water flows from hand basin taps can influence infection spread in aged care...
What are the benefits of an RSV vaccine for older adults?
Research suggests that vaccination against respiratory syncytial virus for adults over 60 has a...
Aged care antibiotic could put residents at risk
Better antibiotic management is needed in residential aged care to protect against...